'Big beautiful bill's' ugly reality for American healthcare
Trump’s “Big Beautiful Bill” will cut federal spending, reduce coverage, and restructure Medicaid, triggering major economic, medical, and social consequences.
-
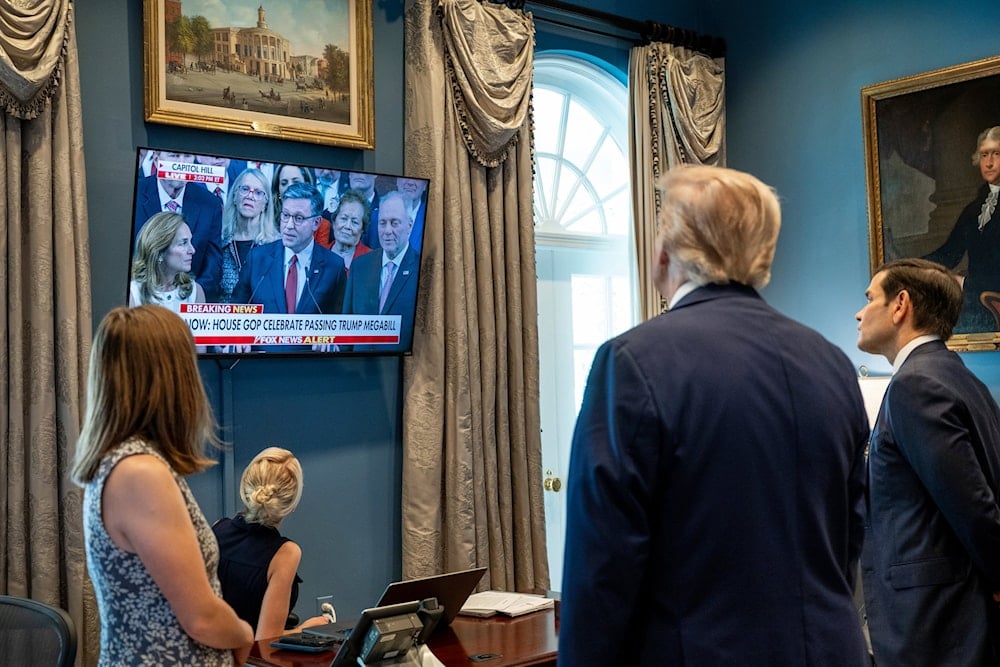
IUS President Donald Trump and Secretary of State Marco Rubio watch Speaker of the House Mike Johnson on television in the Outer Oval Office of the White House in Washington, after the House passed the "Big Beautiful Bill," Thursday, July 3, 2025 (White House via AP)
US President Donald Trump's "Big Beautiful Bill," officially the One Big Beautiful Bill Act, marks a seismic shift in US healthcare legislation. Signed into law on July 4, 2025, this sweeping policy aims to reduce federal health spending by nearly $1 trillion over a decade.
In doing so, it delivers one of the largest Medicaid cuts in American history, sets strict new eligibility requirements, and reconfigures insurance markets, effectively transforming the American healthcare system.
Coverage reductions, medicaid cuts
According to the Congressional Budget Office, the bill is projected to strip 11.8 million Americans of health insurance by 2034, with estimates rising to 17 million under broader policy effects.
Beginning in 2026, able-bodied Medicaid recipients aged 19 to 64 must complete 80 work hours per month to retain coverage. Additionally, eligibility checks will shift from annual to biannual, increasing the risk of coverage loss due to administrative errors.
Financial impact on hospitals, insurance
Hospitals face unprecedented financial stress. Medicaid payments will be slashed by $665 billion over the next decade (18.2% reduction), while uncompensated care costs are expected to soar by $84 billion in 2034 alone.
Rural hospitals are particularly vulnerable, with over 300 at risk of closure. States like Missouri and Kansas face 29% and 15% Medicaid funding reductions, respectively. The legislation caps state-directed payments that many hospitals rely on for financial survival.
Insurance market instability
The coverage losses create dangerous adverse selection dynamics. As healthy individuals drop coverage due to work requirements and barriers, insurers are left with sicker, costlier populations.
Industry analysts project that the combination of healthier individuals leaving the market and sicker individuals remaining could drive premium increases of 15–25% annually in affected markets. Premiums, the monthly payments people make to keep their health insurance active, could rise dramatically as insurance companies face costlier patient pools.
Analysis by KFF, a nonpartisan health policy research organization, shows that premiums could rise by an average of 75% for remaining enrollees as healthier individuals exit the market. "The concern is that you create unstable insurance markets where only the sickest people can afford to stay in," explains Cynthia Cox of KFF. This creates a feedback loop where each round of premium increases pushes more moderately healthy people out of coverage, accelerating the adverse selection.
Human, economic consequences
Studies conducted by researchers at Yale University and the University of Pennsylvania project severe mortality impacts resulting from the loss of health coverage, totaling over 51,000 annual preventable deaths. An estimated 11,300 deaths could occur annually due to 7.7 million people losing Medicaid coverage, while 8,811 deaths are projected from 5.1 million losing Affordable Care Act (ACA) marketplace coverage. Additionally, the elimination of prescription subsidies for Medicare beneficiaries could lead to 18,200 deaths, and the repeal of nursing home staffing standards could result in 13,000 deaths.
Republicans are celebrating the passage of the largest Medicaid cut in U.S. history to pay for the largest tax break for billionaires in American history.
— Bernie Sanders (@BernieSanders) July 3, 2025
51,000 Americans will die each year so that the top 1% can get a $1 trillion tax break.
This bill is a death sentence.
Workforce productivity, medical debt
The labor market will also be affected by the healthcare cuts as every 10% increase in health insurance costs reduces hiring by 1.6%. Uninsured workers miss twice as many work days due to illness, costing employers $575 billion annually in lost productivity. With over 530,000 Americans already filing bankruptcy annually due to medical bills and one-third of credit card debt stemming from healthcare costs, the medical debt crisis in the US will only intensify.
-
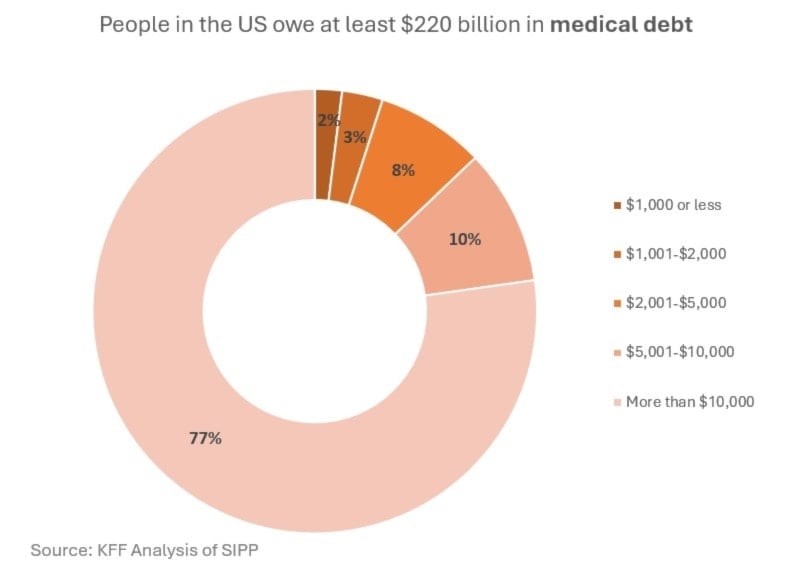
77% of Americans owe more than $10,000
State-level budget shortfalls
States will receive $1.3 trillion less in Medicaid funding over ten years. New caps on provider taxes reduce state flexibility to finance healthcare safety nets. Expansion states like Montana, Arizona, and Kentucky face up to 21% in funding cuts.
Timeline to implementation, political backlash
Major changes are phased between 2026–2028 to minimize immediate political backlash, but enhanced ACA subsidies expire on January 1, 2026, providing Democrats with immediate campaign material for the 2026 midterms.

 4 Min Read
4 Min Read










